The Government of Peru has decided to declare a health alert before the possible arrival of cases related to monkeypox, as a preventive measure against the registration of the disease in various parts of the world, explained this Thursday the Minister of Health of Peru, Jorge López during a press conference.
“We are declaring the alert. We should be generating it tomorrow. In our country we do not have any cases, but the alert is being declared to prevent any eventuality», said the minister, who urged citizens to maintain preventive care.
Since last May 7, in Europe, the presence of monkeypox has been detected. That day, the United Kingdom sounded the alarm and warned of the first case on European soil. Over the days the registered cases have risen to nine.
Then came the turn of Portugal, which confirmed five cases and is keeping a score under study. While in the middle of this week, it was Spain that reported that it was investigating eight suspected cases, which have finally become seven confirmed and 22 are under study.
The Swedish Public Health Agency has also warned of a confirmed case in the Stockholm region. Outside Europe, in recent hours it has emerged that a case has also been detected in the state of Massachusetts in the US. This is a man who had recently traveled to Canada.
It is a very rare infection, which had rarely been detected on the European continent, almost always linked to trips to the African continent, where the infection had been contracted. Here is what is known about this disease.
Wasn’t smallpox eradicated?
Yes, smallpox is a disease that has been considered eradicated for 42 years. It plagued humanity for several millennia, decimating the world’s population on several occasions. It is estimated that in the 20th century alone, it killed around 300 million people.
At the end of the 18th century, the first modern vaccine against smallpox was created, but it was not until the 1960s that massive vaccination campaigns were launched. The last case of naturally contracted smallpox occurred in 1977 and in 1980 the World Health Organization (WHO) certified its global eradication.
The pox of monkeys is caused by another virus, the ‘monkeypox’, although it belongs to the same family as the virus that caused smallpox in humans, the variola virus.
When was monkeypox first detected?
Monkeypox was first detected in 1958 in monkeys used for laboratory testing. Subsequent investigations found that other animals also carried this virus, such as rabbits and mainly rodents, such as squirrels, rats and mice, which are considered the main reservoir of the virus.
However, the infection of a human by this virus was not described until a few years later, in 1970, in the Democratic Republic of the Congo, the country in which most of the recorded outbreaks have occurred since then.
Is it only registered in Africa?
Monkeypox is considered an endemic infection in part of the African continent, specifically West and Central Africa. However, in recent times the scientific community has begun to worry about its spread.
Currently, one of the countries that registers the most cases annually is Nigeria, paradoxically one of the most developed and richest countries on the continent. The country has registered 558 cases of this disease in the last five years, which have caused 8 deaths, according to the latest report from the Nigerian Center for Disease Control (NCDC).
Until the beginning of this month, there was no evidence of its spread in Europe, until the United Kingdom sounded the alarm. The case registered on May 7 corresponds to a patient who had traveled to Nigeria.
Prior to the cases that have occurred in recent weeks, this disease had only been documented in four countries outside of Africa: the US, the UK, Israel and Singapore. The last time was in July of last year in the American county of Dallas, in a country (The US) that had not registered a case since 2003.
How does the virus ‘transit’ between animals and humans?
The initial infection of humans occurs when they come into close contact with animals that have the virus in jungle areas or with their contaminated meat. This contagion is estimated to be unusual and limited.
On the other hand, transmission between humans occurs when contact is made with liquids, mucous membranes, excretions or saliva of the person who is infected by the virus. So the infection could also occur by viral excretion through feces and by having sexual intercourse, as well as through the placenta from the mother to the fetus.
So far, the longest chain of transmission that has been documented in a community reached six successive infections from person to person.
What are the human symptoms of monkeypox?
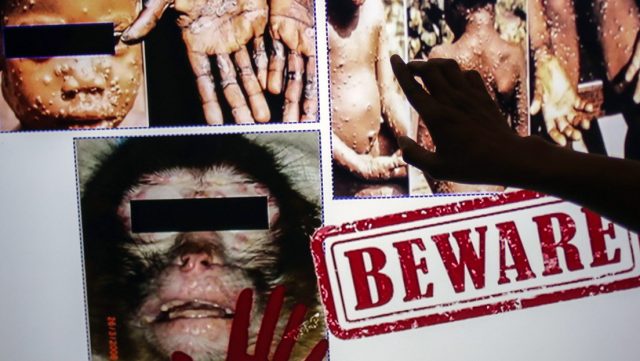
The symptoms that this disease presents in humans are similar to those of the eradicated smallpox, although milder, and begin to develop around 6 to 13 days after the infection has occurred, although the incubation period can vary between 5 and 21 days.
The first symptoms are fever, headache, tiredness, muscle and back pain, as well as swollen lymph nodes. This last symptom is one of those that differentiates it from smallpox, in which lymphadenopathy is rare.
Between one and three days later, a rash begins to appear, which usually begins on the face and then spreads to other parts of the body. After the face, (in 95% of cases) the most frequent places where these lesions appear are the hands and the soles of the feet, (in 75%) although it can appear in other places, including the genitals.
The rash takes the form of fluid-filled bumps that go through different phases until they crust over and eventually fall off. On average, the disease lasts between 2 and 4 weeks and patients must be treated in isolation units due to their high level of contagion.
Is there a vaccine or treatment?
Currently there is no vaccine for this infection and no specific treatment, beyond those to relieve symptoms.
However, it is known that vaccination against smallpox can be used both before and after exposure and is up to 85% effective in preventing monkeypox – according to the WHO – so people vaccinated against smallpox in childhood may experience milder illness.
The fatality rate of the different outbreaks that have been known since 1970 is between 1 and 11%, the victims being, mainly, young children.
When to suspect having been infected by this virus?
Experts recommend to suspect an infection by this virus when three circumstances come together. The first is the appearance of a rash anywhere on the body with no apparent cause. The second is the appearance of symptoms associated with the disease caused by this infection, from fever to swollen lymph nodes.
The third circumstance that must converge is one of these three: the existence of a link with a confirmed or probable case in the 21 days prior to the onset of symptoms, men who have had homosexual relationships, or have traveled to areas in the African continent where this disease is endemic in the three weeks prior to the onset of symptoms, according to the Spanish Society of Infectious Diseases and Clinical Microbiology.